John Fuller: Well, imagine you’re sitting in a hospital room with your family member, and they’ve been declining for months. Uh, they’re on life support and you wonder if they’ll ever leave ICU. You wonder, “What should we do? Are prolonging the inevitable?” This is Focus on the Family with your host, Focus president and author, Jim Daly, and I’m John Fuller.
Jim Daly: John, that’s a heart-wrenching situation. No one can prepare for it. Um, you know, you don’t do this over and over again. These are one-time events sometimes, where your loved one is in difficulty, and you don’t know what to do sometimes. 100 years ago, most people spent their final days at home. That was normal. Uh, today I think only about 20% will, uh, die in their home. Most of them are in ICU or in hospice or in some other facility to take care of them.
John: And if you’re not really a medical expert, there are so many overwhelming, uh, options for decisions. Um, there are ventilators, feeding tubes, dialysis. Um, technologies are, are abounding. And what do you do to help, uh, that spouse or loved one?
Jim: Eh, John, that’s so true. And then you look at the COVID situation, uh-
John: Hm.
Jim: … these decisions have become even more difficult. Uh, we had staff members who tragically, uh, were barred from visiting their loved ones at the end of their lives and weren’t with them to hold their hand and be present as they went from this life to the next.
John: Yeah.
Jim: Uh, today we’ll hear from a medical expert, I’m so glad that, um, she is with us to talk about these things. Don’t pull back. Don’t, uh, go off the YouTube channel, don’t turn off the station, don’t close the app, these are really important discussions to have.
John: Mm-hmm.
Jim: And I think it’s one of the unique ways Focus on the Family is here to help you think about these things.
John: Yeah, and our guest is Dr. Kathryn Butler, uh, a former trauma surgeon with a decade of experience in critical care and, uh, she has a, a really terrific book that, uh, can help you think through these difficulties. It’s called Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care. And we have copies of that here, call 800, the letter A, and the word, FAMILY. (800) 232-6459 or stop by focusonthefamily.com/broadcast.
Jim: Dr. Butler, welcome to Focus on the Family.
Dr. Kathryn Butler: Thank you so much for having me, it’s a real privilege.
Jim: Now, I’m looking at you thinking, “Wow, this could be my daughter.” (laughs)
Dr. Butler: Yeah, I know.
John: (laughs)
Dr. Butler: (laughs)
Jim: And you’re a doctor. You were a trauma surgeon for 10 years.
Dr. Butler: I look like Punky Brewster, I know.
Jim: (laughs)
John: (laughs)
Dr. Butler: (laughs)
Jim: You just look so young, it’s amazing. And, uh, but, man, you accomplished so much. Give us a little bit of your background to help the listeners, understand, uh, where you’re coming from, your experience.
Dr. Butler: Sure. Sure, so, I completed my medical school training at Columbia. I went on to train in general surgery and surgical critical care, which is ICU care, uh, at Mass General Hospital, and then I joined the staff. And was involved in, um, taking care of patients after trauma in the emergency room and basically any kind of emergency-
Jim: Mm.
Dr. Butler: … that brings you into the ER, for which you need urgent surgery.
Jim: Right.
Dr. Butler: That was my role. And then I was also, uh, a specialist in taking care of people in the ICU.
Jim: In that context, I mean, medicine has made remarkable gains.
John: Mm.
Jim: I mean, you can measure them almost every couple years-
Dr. Butler: Mm.
Jim: … there’s some great advancement that occurs.
Dr. Butler: Mm.
Jim: And being a scientist and being a doctor, um, this has brought some, uh, confusion, let me use that term, into end-of-life issues. So, uh, uh, from that perspective, how did you see that first-hand experience as a trauma doctor?
Dr. Butler: Oh, y- you know, and, and what you allude to, the fact that these measures are actually a gift from God, and they allow us, in the right circumstances, to usher people back to health. That’s actually what drew me to the field. I can remember when I was on my pediatric surgery rotation as a medical student, we had this, uh, one little boy who was brought in after being kicked in the abdomen by his mother.
John: Mm.
Jim: Uh.
Dr. Butler: Uh, and he suffered a crack to his pancreas.
Jim: Mm.
Dr. Butler: And I watched in the ICU as he, in the setting of this, had so much inflammation surging throughout his body that his extremities ballooned up and his kidneys started to fail, and his lungs were failing. And so, I helped with the ICU team, as a student, I didn’t do much, but I witnessed how ventilators, and vasopressors, and all these things we use in the ICU that are very aggressive and intensive helped to keep him alive long enough for him to go to the operating room-
Jim: Ah.
Dr. Butler: … where his pancreas was repaired. And it was remarkable to see that then a few weeks later I saw him using his IV pole as a scooter down the hallway-
John: Ah.
Dr. Butler: … completely recovered and thought, “Wow, this is just an incredible way to help people.”
Jim: Yeah.
Dr. Butler: But then over the course of my time actually working as an attending in the unit, what I would see so often was that these measures that when we use them with discernment for people who have recoverable illness, right, so what’s making them so sick is something that we can fix, pneumonia and we have the right antibiotics for it, a heart attack and we can open up the blood vessels with the stent, then these measures would help. But for people at the end of life, who were in… actively dying, who had, uh, multiple medical issues that they were in their end stages, and already causing some degree of organ failure, and for which we had no treatment, these measures would prolong death, cause suffering, and just pitch families into some agonizing situations-
Jim: Mm.
Dr. Butler: … over wondering what to do. And what I saw too was that, appropriately, so many of us we’re in… when we’re in these scenarios, lean into our faith. And we try to say, “Okay, what does the Bible teach me, what would God want me to do?” But the reality of what we see at the bedside with all this machinery is so far removed from the truths that we c- proclaim every Sunday in church, that we really struggle to reconcile-
John: Mm.
Jim: Yeah.
Dr. Butler: … our faith and what we know of Christ and the hope we have with numbers on a monitor that are indecipherable.
Jim: Right.
Dr. Butler: And so, it just puts people into so much confusion-
Jim: Yeah.
Dr. Butler: … and grief-
Jim: Yeah.
Dr. Butler: … and anguish.
Jim: Let me ask you about that, I mean, it rolls right to my next question, many families aren’t sure if, if their loved one is recovering or dwindling at that state, right. We’re talking mostly end-of-life scenarios here.
Dr. Butler: Mm-hmm.
Jim: And it can confuse people. And sometimes the doctors aren’t extremely helpful.
John: Hm.
Dr. Butler: Right.
Jim: Um, they’re moving pretty fast, they’re looking for directives, they’re looking for things that the family or the, the person lying in the hospital bed had declared beforehand.
Dr. Butler: Right.
Jim: W- eh, what have you seen in that regard, that confusion you’re talking about? And, and what about is this recoverable or is this helping the person end well?
Dr. Butler: Yeah. The, the problem is that from the doorway, it’s impossible for a layperson to see if someone who’s o- in the ICU, on this level of care is recovering and on the verge of coming off everything and going home, or actually is dying. There’s no way for them to tell that from the doorway.
Jim: Yeah.
Dr. Butler: Uh, because people in this case will both be on a ventilator, they’ll be attached to monitors. They’ll have lots of IV poles, they might even have a dialysis unit at the foot of the bed running continuously. But to be able to understand whether or not all these things are really gonna get someone home or whether it’s just prolonging the inevitable in a pretty awful and cruel way, you need to understand the underlying illness that’s causing this in the first place-
Jim: Yeah.
Dr. Butler: … the trajectory of whether or not people’s organ function is getting better or worse, and whether or not we have any measures that can reverse the underlying illness.
John: Hm.
Dr. Butler: And I think this is really confusing for people, because we don’t explain it as doctors. We really do a very poor job of explaining that life support measures are supportive, they’re not curative. So, if you come to the hospital with trouble breathing and you need a ventilator, whether or not you come off that ventilator is not about the ventilator itself. The ventilator is meant to buy time-
Jim: It’s just doing a function.
Dr. Butler: … and support your lungs until we can reverse the underlying problem. So, if you come in with pneumonia and it’s a simple pneumonia and you are otherwise healthy and robust and we can give you antibiotics and treat the pneumonia, your lungs will recover, and you’ll be off the ventilator in a few days. But if you come into the hospital with respiratory failure from end-stage emphysema that’s not intractable to all of our treatments, plus lung cancer that’s metastatic, plus a fungal pneumonia that’s much harder to treat, that ventilator may keep your lungs going, but it’s not going to reverse your respiratory failure.
Jim: Right.
Dr. Butler: And it’s likely to be something that you eventually pass away on.
Jim: Right.
Dr. Butler: And that’s something that is really hard to understand, coming to the table never having seen this kind of technology before. Um, but I think it emphasizes why it’s so important to have conversations with our doctors-
Jim: Well, that e- I was-
Dr. Butler: … about whether or not these measures are going to save life or prolong death and suffering.
Jim: … Exactly. And I think that’s what I meant in the opening there that-
Dr. Butler: Mm.
Jim: … you know, we don’t encounter these decisions but maybe once or twice in a lifetime, right, for our loved ones.
Dr. Butler: Yeah, right, right, exactly.
Jim: And it’s usually our parents.
Dr. Butler: Yeah.
Jim: Or our grandparents.
Dr. Butler: Right.
Jim: But it, it, it’s not to the point where you y- become proficient at it-
Dr. Butler: Right.
Jim: … as a layperson.
Dr. Butler: Exactly.
Jim: I mean, it’s just that rare and you don’t really go through it and-
Dr. Butler: Right.
Jim: … Let me ask you, uh, you mentioned this, but you encounter families who struggle to apply those Biblical principles-
Dr. Butler: Mm-hmm.
Jim: … in their medical decisions. It sounds like those things are very distinctive, right. Two (laughs) separate-
Dr. Butler: Yeah.
Jim: … kinda categories, but you certainly can be informed by scripture. You had a story in your book a- about a patient’s wife and son who came to different conclusions, w- which I think illustrates the point beautifully.
Dr. Butler: Abso- and this happens so commonly. I, I took care of a gentleman who was in his 80s and my role was to care for him after he had undergone a very intensive surgery. His story over the past year was that he was at the end of life. He was suffering from multiple medical conditions in their end stages, he already had some degree of organ disfunction, and his… he had become so debilitated that the things that normally brought him joy, uh, visiting with his friends, reading the Bible, which had brought him so much solace on a regular basis, exhausted him-
Jim: Mm-hmm.
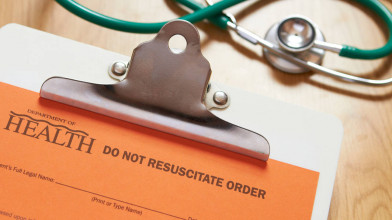
Dr. Butler: … and became laborious. And he underwent this surgery at the behest of his family. He did not wanna undergo it but did it because they urged him to. But he made his wife promise him, “If I decline after surgery, do not let them put me back on a ventilator,” because he had been on one before for a prolonged period of time, found it intolerable, and he said, “I know I’m gonna be with the Lord soon,” and his words to her were, “When he calls me home, let me go home to be with him.”
Jim: Huh.
Dr. Butler: Sure enough, post-operatively, he did develop a pneumonia. We talked with his wife, we talked with his primary doctor, we looked through his advanced directive, which, thanks be to God, he had filled out. And so, it was very clear that even though he couldn’t speak for himself, that if he could answer for himself, he would decline a ventilator. And so, we, we did was we transitioned him to what’s called comfort measures. So, instead of aggressively trying to do all we can to keep someone alive, we instead focus on symptoms. We focus on comfort. We make sure no one’s in pain. We try to make sure that people aren’t struggling with air hunger. And when I left that evening, his wife was holding his hand, speaking to him softly, and said to me, “Thank you, I know he’ll be with, with the Lord.”
Jim: Mm.
Dr. Butler: You know, and so, she was at peace a f- in what was a horrible situation.
Jim: Sure.
Dr. Butler: A few hours later, their son, from whom they’d been estranged for many years-
Jim: Oh.
Dr. Butler: … arrived in the hospital furious with our decision. And he stormed into the ICU room and threatened to call the police if we didn’t put his dad on a breathing machine. And he addressed his father’s Christian faith to justify his argument. And said, “My dad was a Bible believing Christian who went to church every Sunday until his sickness prevented him from doing so. He would not be okay with this, you’re killing him.”
Jim: Huh.
John: Hm.
Dr. Butler: And the, the hear- I… this scenario was so heart-wrenching, but I think it demonstrates what we see so often, is that the landscape is so familiar, and the situations are so highly emotionally charged that people will try to draw from their faith to inform their decisions, but you had this situation where the wife was resting in the sovereignty of God-
Jim: Right.
Dr. Butler: … also seeing her husband as an image bearer of God and sticking to honor his wishes, and the son drawing from the sanctity of life. Those are all Biblical principles, but they arrived at diametrically opposed conclusions.
John: Mm.
Jim: Yeah.
Dr. Butler: You know, so even while we try and struggle to say, “I wanna be God-honoring in whatever I do. What does the Bible allow me to do?” We can really falter, because the situation is so foreign and unfamiliar.
Jim: A- And what happened, what was the story there?
Dr. Butler: So, we had a long discussion with him and tried to discuss with him the fact that even though, yes, the Bible calls us to protect life, but it… the sanctity of life and a need to protect it also doesn’t refute the inevitability of death and that it will come to all of us.
John: Hm.
Dr. Butler: And his dad was at that point where anything further that we did was not gonna bring him home to a life where he could pray, and read the Bible, and commune with friends, he was, he was in organ failure, and we were likely just to prolong his suffering, and he very clearly stated that that was not acceptable for him.
John: Hm.
Jim: Wow.
Dr. Butler: You know, so, we had a discussion, but we upheld the wishes that we could perceive his father would’ve-
Jim: Yeah, no, that’s important-
Dr. Butler: … wanted.
Jim: … to know.
John: Well, we’re talking about some tough stuff, some gray areas, but, uh, through the lens of, uh, a Christian filter, if you will, um, a Christian perspective of what the Bible might say, uh, Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care is the book we’re discussing. Dr. Kathryn Butler is our guest on Focus on the Family. Reach out to us if you’d like a copy of that book. It is, uh, a really essential resource for you and your family.
Jim: Uh, Dr. Butler, y- you offer four Biblical principles, I think the time is right to kinda get into those-
Dr. Butler: Sure.
Jim: … so we can unpack them, um, to guide families through difficult decisions. First, the, the Bible teaches that human life is sacred, you’ve touched on that. How have you seen people, uh, misapply-?
Dr. Butler: Mm.
Jim: … what you’re saying there?
Dr. Butler: Mm-hmm.
Jim: I think it’s important for us to learn from that.
Dr. Butler: Sure, sure. So, first, before I dive into the principles, I need to emphasize that they’re dynamic. I think a lot of times we stumble on these situations, when we cleave to one of them without looking at the whole Biblical narrative and that we are fallen in sin, redeemed in Christ.
John: Hm.
Dr. Butler: And, and that we are made for the Lord. (laughs)
Jim: I want you to be my doctor.
Dr. Butler: (laughs)
John: (laughs) Yes.
Jim: I like this.
John: Yes.
Dr. Butler: I would love to.
Jim: (laughs)
Dr. Butler: I’m homeschooling my kids right now-
Jim: Yes, yes.
Dr. Butler: … so you might take that back.
Jim: Yeah.
Dr. Butler: (laughs)
John: Just make sure you’re in Boston when you need her.
Dr. Butler: (laughs)
Jim: There you go.
Dr. Butler: Um, you know, so, I, I think it’s important that we not hone in on just one-
John: Hm.
Dr. Butler: … but we really consider them all together. And the first, as you mentioned, is, yes, that mortal life is sacred. Uh, we are all made in God’s image and have inherent dignity and value. And God gives us life as a gift for us to steward.
Jim: Hmm.
Dr. Butler: Um, and, you know, the sanctity of mortal life, which takes us back to Mount Sinai, and the 10 Commandments, and the mandate to not murder, is what also prompts us to protect the unborn, and also prompts us to resist physician-assisted suicide, which is a whole ‘nother topic.
Jim: Yeah, we’ll talk a bit about that later.
Dr. Butler: (laughs) Sure. Um, and in the case of, of end-of-life care, what it should prompt us to do is to accept these kinds of aggressive treatments if there is hope of cure. If what is making us sick is something that’s recoverable. So, the correct question isn’t so much, “Yes, a ventilator, no, a ventilator,” but “A ventilator under what circumstances?”
Jim: Mm-hmm.
Dr. Butler: Um, the second principle, and this is one that I think people can really stumble with, because it seems, at first glance, like it’s in tension with the first, is that even though we are called to protect life, God is still in authority over our life and death. We think about from Isaiah chapter 40, like the grass that is here today, gone tomorrow, so are we, and we are dependent upon the breath of the Lord throughout. And so, even though we are called to protect life, the sanctity of life doesn’t refute the inevitability that death will come to us all.
Jim: Right.
Dr. Butler: And so, as a result, when we are clearly at the end of life, when we’re very elderly and infirm with multiple conditions, that drives us away from care that’s futile. So, and, and it’s important, spiritually, because when we so fight against our own mortality, we actually deny God’s grace and power, and the power of the resurrection.
Jim: Mm.
Dr. Butler: And the truth that he can work through all things, even our death, for the good of those who love him.
Jim: Yeah.
Dr. Butler: Uh, the third one is that we are called to mercy and compassion. You know, we think about the fact that Christ tells us that the second greatest commandment is to love neighbor as ourselves, and Micah tells us that we’re called to act justly, and love mercy, and walk humbly with our God. And when it comes to the end-of-life scenarios that are so hard, that means we need to have concern for the suffering that our treatments inflict. And these matters, because ICU measures do cause suffering. CPR inflicts chest trauma in 90% of cases.
Jim: Hm.
Dr. Butler: Including broken ribs.
Jim: Yeah, it’s not quite what you see on TV.
Dr. Butler: No, it’s not at all. And a, a large m- large proportion of people who suffer through intensive care for a prolonged period of time, struggle with PTSD afterwards, post-traumatic stress disorder.
Jim: Hmm.
Dr. Butler: At rates that are comparable to those suffered by soldiers who fought in the Iraq war.
John: Mm-hmm.
Jim: And that’s just the physical-
Dr. Butler: That’s just from being in the ICU, [crosstalk] having no ability to communicate, being tied down, being stuck with needles constantly. It causes psychological-
Jim: Huh.
Dr. Butler: … trauma.
John: Hm.
Dr. Butler: And, and that’s worth it if we do these things to bring someone home.
Jim: Sure.
Dr. Butler: But if we’re doing this in the setting of someone not going to be able to return, then it looks a lot like cruelty.
Jim: Yeah.
Dr. Butler: And so, part of, of having mercy and compassion is recognizing that these measures cause suffering and not forcing them upon people when that suffering is not without benefit.
Jim: Okay, that’s the third, what’s the fourth principle?
Dr. Butler: And then the fourth is the one that I think supersedes them all, which is our hope in Christ.
Jim: Right.
Dr. Butler: That s- that so vast is God’s love for us, that nothing can wrench us from his love.
Jim: Right, not even death.
Dr. Butler: Not even death.
Jim: Mm-hmm.
Dr. Butler: You know, I, I l- I love Romans 8:38-39 and that’s actually this inspiration for the title for the book, because through Christ, neither life nor death, nor angels, nor rulers, nor anything else in all creation can separate us from his love. And so, while death was never our original purpose, (laughs) and it is wrong, and it’s abhorrent, and it’s the wages of our sin, the cross transforms death from something to be avoided at all cost, to something that promises us hope, because we know that death for us means eternal communion with God-
Jim: Yes.
Dr. Butler: … through the cross.
Jim: Right.
Dr. Butler: And so, while these situations agonize us, we need not sink into despair.
Jim: Mm-hmm.
Dr. Butler: Because we have hope in Christ.
Jim: That is so good. I want to go back and kind of, um, dig into each of the principles-
Dr. Butler: Sure, yeah.
Jim: … if we can do that.
John: Yeah.
Jim: So, the first one, again, was sanctity of mortal life.
Dr. Butler: Mm-hmm.
Jim: You had a patient, uh, nearing death and his son felt obligated to pursue aggressive treatments. Um, describe that illustration.
Dr. Butler: Yeah, he, um, his dad had been in the ICU for a long period of time and was really failing. And we met with his son and, and said, “Listen, you know, your your dad, we’re not gonna be able to get him better. We’re not gonna be able to get him home.” But he was stalwart, because he really thought that the Bible mandated that he do everything at all costs. And I think that’s an easy trap for people to fall into. To think that because we’re called to protect life, we have to always pursue everything.
Jim: Yeah, full measures.
Dr. Butler: No matter the situation. Has to al- that, that full measures are… is always the right answer.
Jim: Hm.
Dr. Butler: And just as a, an aside, this actually plays out in research. What we found is that people with high religious coping, so those of us who go to church and, and look to, um, our spiritual community for solace, actually are less likely to accept hospice care, are more likely to accept aggressive measures during the last week of life and are more likely to die in the ICU.
Jim: Hm.
Dr. Butler: So, we see this, this do everything at all cost mentality. So, he had that initially. And so, we proceeded with everything at all costs. And what that meant was that when his dad had a cardiac arrest, so his heart stopped, we jumped in with CPR, and placed a f- and a breathing tube, and were pounding on his chest and shocking him, and he found it so upsetting to see that he ran into the room and said, “Please stop, he’s had enough.” You know, so, it’s in seeing and believing, on the one hand, that the Christian faith mandates we always do everything and then him seeing the reality of what everything was-
Jim: Yeah.
Dr. Butler: … he, he paused and realized, “This, this might not be the right thing.”
Jim: Mm.
Dr. Butler: So.
Jim: Y- You mention in the book that clinging to medical interventions can, can be a form of idolatry.
Dr. Butler: Mm.
Jim: You’re kinda touching on that.
Dr. Butler: Yeah.
Jim: But let’s just put it on the table. Is that idolatry to try so hard to avoid death?
Dr. Butler: It, it can be if we are clinging to medical technology as the answer irrefutably.
Jim: Huh.
Dr. Butler: And not considering that the Lord is sovereign even over this technology. And, and I say that thinking about people, which is very common, who will say, even against their family’s wishes, say, you know, “I, I, I know my mom would not want a ventilator right now and would not want all these aggressive things done, but I’m praying for a miracle.”
Jim: Yeah.
Dr. Butler: Which is a very understandable thing, you know, as someone who’s following Christ, to say. And say, uh, you know, “I know God can do all things, so I’m just praying for a miracle.”
Jim: Yeah.
Dr. Butler: But the thing is, God doesn’t need our ventilators, you know. A miracle by definition is something that’s beyond our natural means that he does just out of his mercy.
Jim: Mm.
Dr. Butler: And so, we can pray for a miracle, but when we decide that we’re gonna continue technology that causes suffering against someone’s wishes and hoping that he will perform that miracle-
Jim: Yeah.
Dr. Butler: That, that veers toward idolatry, ’cause we’re clinging so tightly to this technology instead of resting in-
Jim: Yeah. And it does-
Dr. Butler: … our trust in the Lord.
Jim: … th- this bigger issue, and I think that’s principle two, God’s authority over life and death, um, that bigger principle of how technology can prolong the inevitable.
Dr. Butler: Yeah.
Jim: And then w- where do we as Christians begin to say, “We’re relying on technology-”
Dr. Butler: Right.
Jim: “… and not God.” I have family members who-
Dr. Butler: Hm.
Jim: … have been diagnosed with cancer and, y- you know, th- they go in… they’ve gone in different directions. One is saying, “You know what, I don’t want the chemo, it’s gonna-”
Dr. Butler: Mm-hmm.
Jim: “… cause me, uh, difficulty with, uh, end of life.”
Dr. Butler: Mm-hmm.
Jim: “It’s not gonna be a, a good quality end of life, that’s their decision.”
Dr. Butler: Mm-hmm.
Jim: So, they’re gonna go into a glide path and die with the cancer.
Dr. Butler: Mm-hmm.
Jim: Or die from the cancer.
Dr. Butler: Mm-hmm.
Jim: And then others that are more aggressive and really going after it. Speak to that, um, you know, sometimes the treatments, as you’re saying, can be very destructive-
Dr. Butler: Mm-hmm.
Jim: … to your quality of life.
Dr. Butler: Mm-hmm, mm-hmm.
Jim: And, um, I think there’s a book out, it’s not a Christian book, called Being Mortal.
Dr. Butler: Yeah.
Jim: And it speaks to that issue-
Dr. Butler: Yeah.
Jim: … of how you need to assess the cost-
Dr. Butler: Mm-hmm.
Jim: … of that aggressive treatment and what it’s gonna do to you.
Dr. Butler: Right. Right, absolutely. And, and what you’re honing in on too is that suffering is something that’s subjective. And so, what may be suffering for one individual is not for another. And so, our answers to this will vary, it’s just important that we consider them ahead of time.
Jim: Right. And I don’t mean to offend anybody.
Dr. Butler: No.
Jim: ‘Cause those are very personal decisions-
John: Yeah.
Jim: … obviously.
Dr. Butler: Yeah, exactly. And I think as unique image bearers of God, we are all gonna have our own v- you know, backstories and dis- or our understandings of what we can tolerate, what’s meaningful to us, what really matters. And so, our answers are going to vary.
Jim: Yeah.
Dr. Butler: And so, it… when we’re having these discussions with family members, it’s critical to sit down and to think about what matters to me. When I look back at my own history and as I consider my own walk with the Lord, what’s okay and what’s not.
Jim: Yeah, and that’s so good.
Dr. Butler: And the answers are gonna differ.
Jim: Yeah. And, uh, it’s the reason we wanted to do this broadcast with you.
John: Mm-hmm.
Dr. Butler: Mm-hmm.
Jim: To inform people to be thinking about these things. L- Let’s end with scripture.
Dr. Butler: Sure.
Jim: You’ve done a wonderful job-
John: Yeah.
Jim: … weaving in the scripture to the discussion today. And we’re gonna have you come back tomorrow-
Dr. Butler: Sure.
Jim: … if you can do that.
Dr. Butler: Absolutely.
Jim: Um, in Philippians 1, Paul says his reason for persevering, and I think this is really good, persevering is to serve God.
Dr. Butler: Mm-hmm.
Jim: Um, and you speak to that in your book about if the reason you want to continue is that you c- have enough quality of life to continue to serve the Lord-
Dr. Butler: Amen.
Jim: … that’s, like, the number one goal, right.
Dr. Butler: Right, right.
Jim: Uh, speak to that and how you can apply that passage in an end-of-life decision.
Dr. Butler: Yeah. So, and we’ll talk about, um, advanced directives, but I, I would just encourage as you’re thinking about these topics, which are so hard and no one wants to think about them, but it’s important, to think about the moments in your life when you have known, like from the Westminster Catechism, “Our ch- the chief end of man is to know God and enjoy to him forever, to glorify God and enjoy him forever,” when have you been able to live that out? Has it been when you’ve been able to pray and read the Bible? Has it been when you’ve been able to serve? When you’ve been able to love on your family members? What are those things that are crucial to you in your walk with him? And help that to guide you.
Jim: Yeah.
Dr. Butler: And sometimes the answers are simpler as a result.
Jim: Yeah. And, Katie, it’s so hard for us on this side of eternity to think of these 80, 85 years, if we’re blessed with that-
Dr. Butler: Yeah.
Jim: … to not feel like that’s the whole enchilada.
Dr. Butler: Mm-hmm.
Jim: But we’re talking about eternity.
Dr. Butler: Right.
Jim: Right?
Dr. Butler: Right.
Jim: There is so much that’s gonna happen after this.
Dr. Butler: Right.
Jim: In the presence of God and being in Heaven with him-
Dr. Butler: Yeah.
Jim: … for eternity.
Dr. Butler: Yeah.
Jim: It’s hard to wrap your mind around that and to not be fearful that this is it.
Dr. Butler: Right.
Jim: This is all I have. Guess what, this is not all you have as a Christian.
Dr. Butler: No.
Jim: And that’s what excites me. Thank you for opening this discussion up and having it with us today. And we will have you come back tomorrow. We’ll continue to talk about advanced directives and some other things that people need to know about. Um, yes, this can be a painful topic, but I hope, I hope we’re conveying the spirit of discussion in this regard, to help equip you to have the most information possible to make good decisions. And if you’re in that place where you’re a caregiver for an elderly grandparent or parent or someone in your life and you don’t know what to do, call us. We’ll be able to help, uh, give you some input. We have caring Christian counselors that can help.
John: Mm-hmm.
John: Mm-hmm.
Jim: It’s free of charge, we’re not gonna charge you for that. Um, I’d love to invite you to come into ministry with us, and if you can make a gift of any amount to Focus, we’ll send you, uh, Katie’s wonderful book on a tough subject called Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care. Uh, we’ll send that to ya as our way of saying thank you.
John: Mm. Reach out to schedule a time to talk to one of our counselors or to donate and get this, uh, great resource, Between Life and Death, uh, the number is (800) A-FAMILY, or stop by focusonthefamily.com/broadcast. On behalf of Jim Daly and the entire team here, thanks for joining us today for Focus on the Family. I’m John Fuller inviting you back as we once again help you and your family thrive in Christ.